Lambeth Living Well Collaborative
The Lambeth Living Well Collaborative was established in June 2010. The collaborative is a platform of partners who have come together to radically improve the outcomes experienced by people with severe and enduring mental health problems. The Collaborative is made up of people who use services, carers, commissioners across NHS Lambeth Clinical Commissioning Group and Lambeth Council, voluntary and community sector, secondary care and primary care. The vision of the Collaborative is that 'the Lambeth Living Well Area will provide the context within which every citizen whatever their abilities or disabilities, can flourish, contribute to society and lead the life they want to lead'.
The Collaborative is aiming to enable people in Lambeth to achieve the following 'Big Three' outcomes:
- Recover & Stay Well: experience improved physical and mental health.
- Choose: experience increased self-determination and autonomy.
- Participate in daily life on an equal footing with others and specifically:
- To 'connect' with family, friends, neighbours.
- To 'give' in the community through community activities, volunteering or peer support.
- To be included in society with reduced stigma and discrimination, especially in relation to mainstream services such as education, employment, and housing.
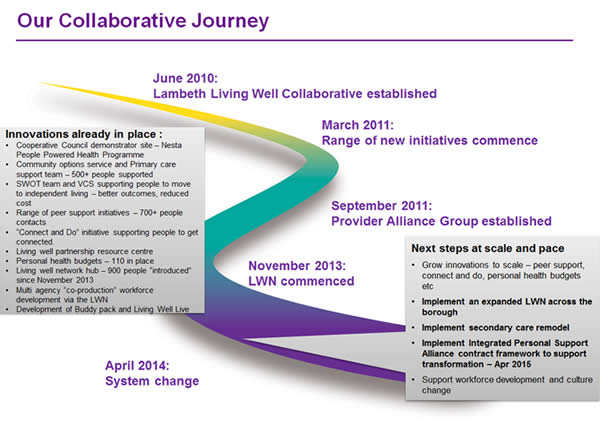
This image shows the collaborative journey since June 2010:
What was the issue and whose idea was it to do this?
Lambeth is a central London Borough of 300,000 residents which has nearly three times more people registered with severe mental illness than the national average .
The collaborative was set up by commissioners, service users and providers in response to a range of challenges including the very poor outcomes experienced by people with serious mental health problems; concern that the system of care was overly medical and too dependent upon "beds"; that support was not being provided early enough to avoid crisis. In addition there was awareness of significant funding reductions especially within social care (40% reductions from 2014/15) but also efficiencies required within the NHS. In brief partners agreed that we needed to transform from an overly crisis-dominated system to improve the quality of outcomes for people using services and focus on prevention and early intervention. They felt this could be possible if they made better use of the skills and insight of people who use services and organisations that provide them.
Who is involved and what are they contributing?
The collaborative includes organisations from health and social care (GPs, the wider NHS, the local authority and community based health services) and voluntary sectors. Collectively their work is focused on supporting people in Lambeth to live well with their mental health. Peer supporters, service users and their advocates are involved in the Collaborative in co-designing new services and reviewing existing provision. The road map sets out the key objectives that the collaborative wants to achieve - this has been developed in large group sessions. Regular breakfast meetings, which are open to all, take decisions about the day to focus of work and refine and adjust the immediate work to respond to changing local circumstances.
A Provider Alliance Group was formed during 2012 to help deliver the evolving service offer. This brings together primary care, the voluntary and community sector, social care, secondary care, service users and commissioners. Its main priority has been to develop and deliver the Living Well Network, Lambeths new 'front door' for people with mental health problems seeking help and support.
How are people with lived experience involved?
The Collaborative support a whole range of organisations that have Peer Support initiatives including Mosaic Clubhouse (opens new window), Thames Reach (opens new window), Certitude (opens new window), Look Ahead (opens new window), Mind (opens new window), South London and Maudlsey NHS Foundation Trust (SLaM). (opens new window) People with lived experience have been part of the co-designing and commissioning of services in Lambeth and play a constant role in strategic decision making.
Much of the work is targeted specifically at building on the insight of people with lived experience. For example, the Peer Innovation Fund was developed by the collaborative in 2013. It is a strategic fund open to people with lived experience of services. The fund is focused on finding more ways to develop peer support in the borough. People submitted ideas and those that were shortlisted then received financial support, training and skills development to turn their ideas into projects. Some of the projects developed so far include;
- Project Dare: a group intervention that challenges stereotypes of womens body image, increases self-esteem and teaches self-compassion whilst celebrating the body and having fun. Sessions are planned and facilitated by someone who has experience of mental ill-health.
- Recovery in Action: a personal development project for people with a lived experience of active addiction and/or mental and emotional turmoil led by someone with a lived experience of addiction.
People with lived experience are involved in all stages of the commissioning process; from co-designing the service specifications through to taking part in tender panels alongside commissioners.
How are decisions made?
The collaborative meets for breakfast once a month. These are open sessions that people with lived experience regularly take part in. These sessions do generally maintain a broad representation but it is recognised that this forum doesn't always work for everyone. The collaborative is focused on maintaining a wide range of mechanisms for engagement including group meetings, peer support network meetings that feedback into breakfast sessions plus an increasingly strong online communication and feedback tool that is managed by Mosaic Clubhouse. Within these sessions progress is reviewed and new strategy is developed. Agreeing and updating the 'Road map' for the collaborative is also a key output for some of these sessions
The Collaborative hosts co-design sessions, to which over 1,800 people from the Borough have actively contributed. For example in September 2014 a session was held on taking an asset based approach. The workshop aimed to ensure a common understanding of this language and to make plans to take things forward in Lambeth. External speakers shared lessons and practice from elsewhere followed by roundtable sessions to develop ideas for Lambeth.
What has it cost? Who's contributing what resources?
The collaborative agreed from the very beginning that it was important to be completely transparent about its costs. This was to help build people's understanding of the work they are doing and to build trust between everyone involved. They created the resource map to be clear about what money is currently within the system and where it is spent.
There has been no new or additional budget for the Collaborative. All of the work that has taken place is funded through existing commissioning budgets. In some areas, like aspects of secondary care, the collaborative identified that services were not supporting their aims. That funding has now been used to re-commission different types of provision that have been co-designed with people with lived experience.
What processes and methods are you using to get this work done?
Commissioners have used practical methods, such as asset mapping and prototyping new ideas (AAP prototype), to build a more collaborative approach. They have changed some of the technical tools that they use as well. For example, as a result of the relationships that had been developed through the collaborative it became clear that a traditional competitive approach to commissioning services would undermine the collaborative working that had been developed. To address this commissioners are adopting an alliance contracting model. The alliance contracting model enables commissioners to incentivize collaboration and enable integration between providers who each have a unique contribution to make.
In an alliance contract model, a group of providers enter into a single arrangement with the commissioner to deliver services. The key difference is that all parties in the alliance share risk and responsibility for meeting the agreed outcomes. The alliance is not co-ordinated by a prime contractor or provider and there are no sub-contractual arrangements involved. All organisations are deemed equal partners and rely on governance arrangements to manage their relationships and service delivery. The intention is that integration and collaboration are formalised through the contract, as commissioners and providers within the alliance are legally bound together to deliver the specific contracted service, sharing in risks and rewards accordingly.
The types of services that have been developed in Lambeth include peer support services, connect and do, and the Community Options Team. A new service, Solidarity in a Crisis is a telephone peer support service that maintains an active directory of local resources available to the whole community on it's website. A new front door to the mental health system is being built, the Living Well Network (LWN). The LWN commenced in the north of the borough in November 2013 and is being rolled out to the rest of the borough from July 2015. It aims to intervene early to support people before they reach a crisis or to work with people being discharged from secondary mental health services. The LWN brings together primary care, the voluntary and community sector, triage from secondary care, a voluntary sector user led information resource centre and peer support. The plan is to 'open the front door' by encouraging people to self-introduce to services rather than relying on referrals for access. This will take place from July 2015.
What are the outcomes?
There have been over 1,200 introductions (on average 140 per month) to the new "front door" of Mental Health Services - The Living Well Network. This has resulted in a significant reduction in referrals to secondary care since November 2013. This is a reduction of about 50% per month. Over 60% of people who have been supported were previously not know to secondary care services. Over 500 people have been supported within the Community Options Team and Primary Care Support Service. Over 600 contacts have been made with Solidarity in a Crisis, an out of hours Peer Support Service; over 550 people have accessed Connect and Do, an initiative that focus' on building people's confidence and reduce social isolation and 110 people have taken up Personal Budgets.
What have you stopped doing/ replaced/ changed?
Lambeth are slowly reducing the number of acute beds being commissioned as they move away from a crisis orientated approach to one that focuses more on early intervention and prevention. The Clinical Commisisoning Group and South London and Maudsley NHS Foundation Trust have agreed plans to reduce the number of acute psychiatric beds between 2015 and 2017. This is part of a remodelling of secondary care services enabled by a greater focus on early intervention and improved recovery support for people.
As the collaborative is looking at the whole mental health system they have reviewed the various existing services. This has led to several traditional services being decommissioned and then recommissioned in a different way. This means both a different service offer and a different way of commissioning the services. For example the Integrated Personal Support Alliance is a £12 million budget that is currently spent on inpatient care, rehabilitation beds and residential care. This budget is made up of £7 m from the NHS budget and £5 m from Lambeth Council. This is being completely recommissioned to focus on community based support and interventions through an alliance contract. An alliance contract is different to traditional forms of contract as it requires provider organisations and commissioners to collaborate to deliver against a single set of outcomes. The Alliance goes live on 1 April 2015 supported by a (section 75) partnership agreement between Lambeth Council and NHS Lambeth Clinical Commissioning Group. The Alliance agreement includes commissioners and two providers from the voluntary sector, Social care and South London and Maudsley NHS Foundation Trust who will deliver personalised outcomes for people with complex needs. People with lived experience will play a role in the monitoring and evaluation of this work. The key benefits of this approach are improved outcomes for people with complex needs and financial savings of about 20% of the original budget.
